What is HCM?
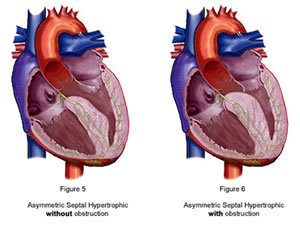
Idiopathic Hypertrophic Subaortic Stenosis (IHSS) is now called Hypertrophic Cardiomyopathy (HCM). It is usually a genetically inherited, slowly progressive disease of the muscle of the heart (cardiomyopathy), which causes thickening (hypertrophy) of the walls of the heart with a specific predilection for hypertrophy of the wall knows as the interventricular septum. The septum anatomically divides the heart’s 2 main pumping chambers, the right and left ventricle from each other. This hypertrophied or thickened septum often results in obstruction of blood flow out of the left ventricular pumping chamber as well as limiting the amount of blood that can flow into the left ventricle when it is filling with blood. Stiffening of the heart’s walls usually develops, which in turn can lead to severe shortness of breath and ultimately can progress over time in some patients to failure of the main pumping chambers to pump or squeeze adequately. This inability of the heart to squeeze or pump forcefully enough is known as heart failure.1. Obstruction refers to the hypertrophy of the interventricular septum as explained above. Below is an illustration of the anatomy of the heart in HCM. The thickened septum gave rise to one of the over 75 names that this disease has had over the years, that being the name -Asymmetric Septal Hypertrophy- or ASH. You will notice in the illustration below that depending on the location and shape of the hypertrophied septum, the anatomy can result either with obstruction of blood flow out of the heart through the aorta (the main artery that carries blood away from the heart) or without obstruction of blood flow to the aorta. When patients do develop obstruction, they often suffer from light-headed spells and even out right fainting spells. This is called syncope or syncopal episodes. Treatment for symptoms related to obstruction consists of cardiac medications which cause the heart to squeeze less forcefully and thereby decrease the amount of obstruction that is present, surgical intervention known as septal myotomy and myectomy, and a procedure known as alcohol septal ablation.
2. Arrhythmias are irregular heartbeats. They are very common in HCM. It is important to note that all people have occasional palpitations or irregularities in the rhythm of their heart. However, some irregular heart- beats are symptoms of true heart disease.
The heart is an electromechanically driven pump. This means that every mechanical contraction or squeeze of the heart is initiated by a prior electrical impulse. In some patients with HCM, there is disease at the cellular level that affects these electrical impulses. When the electrical system of the heart is involved in the disease, patients can have irregular heart rhythms that can vary from arrhythmias that are not life threatening to very dangerous, malignant, life threatening arrhythmias. A common example of the former is called atrial fibrillation, which can still be very frightening in that it causes the heart to race and can make patients with HCM feel light headed, short of breath, and very tired. The more dangerous arrhythmia associated with HCM is known as ventricular tachycardia. Both require treatment with medications at the very least.
The most worrisome complication of HCM is known as “Sudden Cardiac Death.” This can result from ventricular tachycardia progressing on or degenerating into ventricular fibrillation and death. In fact, HCM is the most common cardiac cause of sudden death in young people (30 years of age or younger). However, it should be emphasized that this complication effects only about 1% of the people diagnosed with HCM. When we read about young athletes who die suddenly on our playing fields, undiagnosed HCM is often the cause of these tragic incidents. It should be noted that HCM is not the uncommon disease that it was once felt to be. It is now estimated that HCM effects approximately 1 in every 500 people. It is now possible to identify those people at the highest risk for “sudden cardiac death” and preemptively implant what is called an “ICD” or “Implantable Cardiac Defibrillator” which can recognize dangerous arrhythmias as soon as they begin and immediately shock the heart out of this dangerous rhythm.
3. Compliance refers to the heart’s ability to stretch and fill with blood as much as possible during that part of the cardiac cycle in which blood fills the main pumping chambers or ventricles. It can also be though of as the heart muscle’s ability to be elastic. Some patients with HCM go on to develop a thick stiff heart which has lost it’s compliance or stretch-ability. It therefore fills with less blood before each beat. This loss of compliance is known as “diastolic (filling) dysfunction”. It leads to symptoms of shortness of breath during exercise and fatigue. As of now, there is no good treatment for this complication of HCM.
For more detailed information about HCM, it’s clinical course, and treatment options, visit the Hypertrophic Cardiomyopathy Association (HCMA) website.